Hospital Pricing and Pay for Performance
Ian McCarthy | Emory University
Outline for Today
- Understanding Hospital Pricing
- Recent Pay-for-Performance Programs
- P4P and Prices
Hospital Prices
What is a hospital price?
Defining characteristic of hospital services: it’s complicated!
What is a hospital price?
Lots of different payers paying lots of different prices:
- Medicare fee-for-service prices
- Medicaid payments
- Private insurance negotiations (including Medicare Advantage)
- But what about the price to patients?
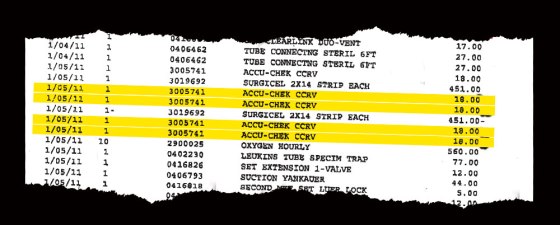
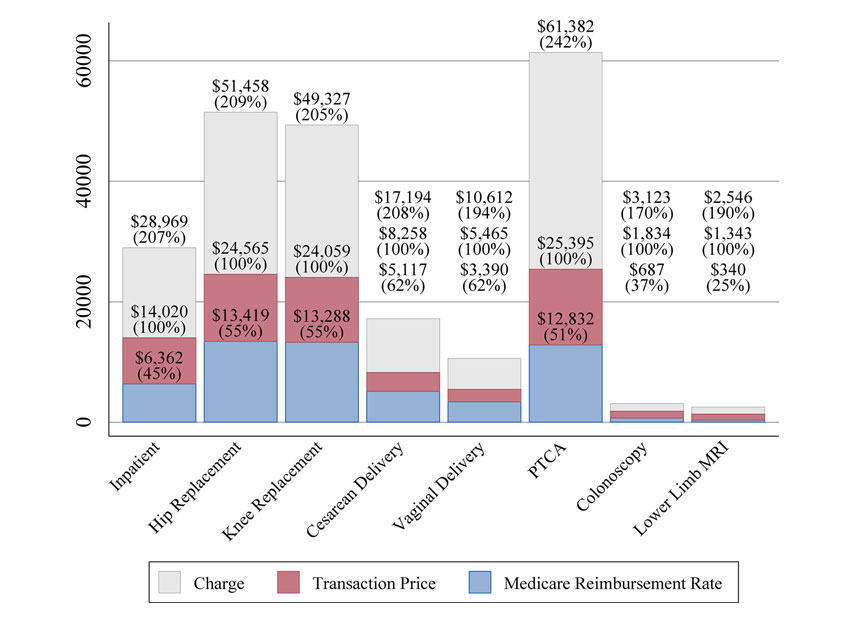
Price \(\neq\) charge \(\neq\) cost \(\neq\) patient out-of-pocket spending
What is a hospital price?
What is a hospital price?
Not clear what exactly is negotiated…
Fee-for-service
- price per procedure
- percentage of charges
- markup over Medicare rates
Capitation
- payment per patient
- pay-for-performance
- shared savings
What is a hospital price?
In most economic discussions, a hospital’s “price” refers to the allowed payment negotiated with insurers. That’s typically the definition I’ll use as well.
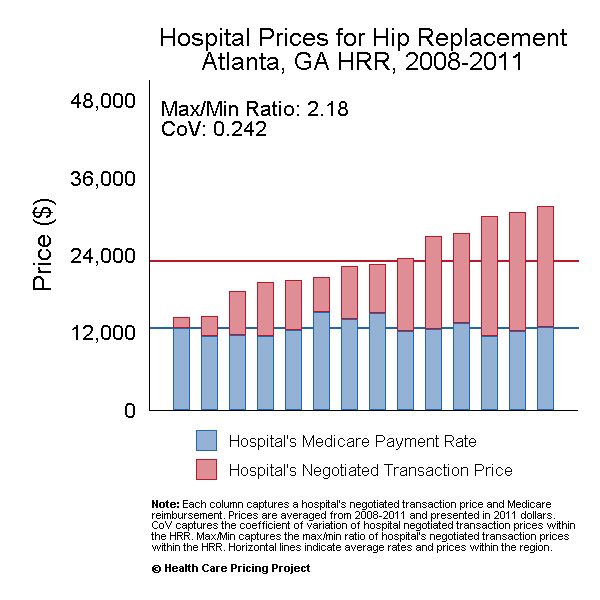
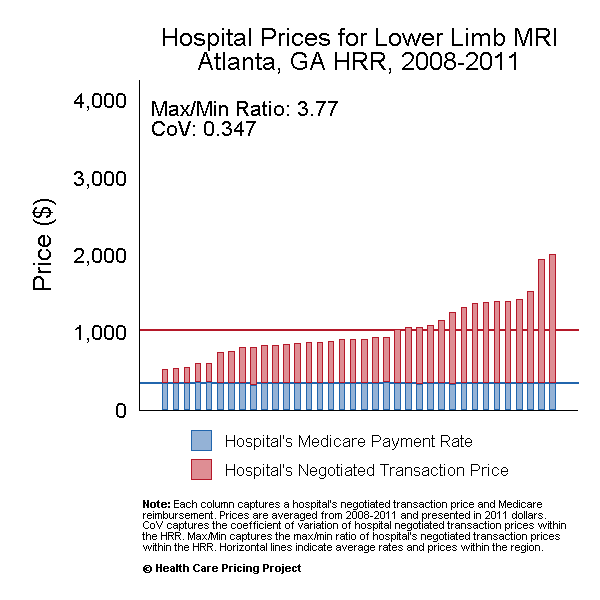
Hospital prices in real life
A few empirical facts:
- Hospital services are expensive
- Prices vary dramatically across different areas
- Lack of competition is a major reason for high prices
Hospital prices in real life
Hospital Pay for Performance (P4P)
Basic Idea
- FFS payments create an incentive to overtreat
- Capitated payments create an incentive to undertreat
- Neither is necessarily a problem unless patient care is adversely affected
Current P4P Programs
There are three main hospital-based P4P programs in Medicare right now, details available here:
- Hospital Readmissions Reduction Program
- Hospital Value-based Purchasing Program
- Hospital-Acquired Condition Reduction Program
HRRP
- Reduces Medicare IPPS payments to hospitals with excess 30-day readmission rates for selected conditions (e.g., AMI, HF, pneumonia)
- Penalties are based on risk-adjusted excess readmission ratios relative to national benchmarks and are capped at 3% of base operating DRG payments
- Purely punitive (no bonuses, only penalties)
- Significant debate surrounding risk adjustment and potential unintended consequences
- HRRP Tracker
VBP Program
- Redistributes Medicare payments across hospitals based on a composite performance score covering clinical outcomes, patient experience (HCAHPS), safety, and efficiency
- Funding is budget-neutral: CMS withholds a fixed percentage of payments from all hospitals and redistributes it based on relative performance, creating both winners and losers
- VBP Tracker
HAC Reduction Program
- Penalizes hospitals in the worst-performing quartile on patient safety metrics (e.g., infection rates, PSI measures)
- Hospitals in the worst-performing quartile receive a flat 1% reduction in total IPPS payments; there are no bonuses
- Blunt, threshold-based incentive focused squarely on inpatient safety and has raised concerns about measurement noise and weak differentiation among hospitals
- HAC Tracker
P4P and Pricing
How?
There are several mechanisms by which P4P programs can influence a hospital’s negotiated price with insurers: - increasing costs - differentiation (e.g., quality improvement or changes in services) - service mix - bargaining
Costs
- P4P may increase real operating costs
- care coordination
- discharge planning
- post-acute management
- If these investments raise costs across all patients, hospitals may seek higher prices from private insurers
Differentiation
- Efforts to reduce readmissions may reflect genuine quality improvements
- Hospitals may position themselves as:
- lower readmission
- better coordinated
- higher value
- Insurers and employers may be willing to pay higher prices for perceived improvements in quality
Service mix
- Hospitals may adjust:
- admissions policies
- intensity of care
- types of services emphasized
- These responses can change the average price observed even if per-service negotiations are unchanged
Bargaining
- Lowering Medicare margins may change hospitals’ incentives in negotiations:
- greater urgency to secure favorable commercial contracts
- less willingness to accept low-price agreements
- Effects depend on relative bargaining power and market structure
- This is a form of “cost-shifting” (although not a mechanical pass-through)
What is Cost-shifting?
- Some concern that when Medicare lowers payment rates, hospitals may respond with higher prices for private-insurance patients
- Is this possible?
- No: If hospitals can unilaterally set prices, they would lower prices to get the marginaly lower WTP patients (not relevant in a bargaining context)
- No: Hospitals must negotiate with insurance companies, and if they could have negotiated a higher rate, they would have done so earlier
- Yes: If profits enter into a hospital’s objective function nonlinearly, then reductions in profit could provide upward pricing pressure
- Policy-makers and hospitals say yes (but for simpler reasons)
- Economists often say no under standard bargaining models, though this depends on assumptions about objectives, constraints, and market structure
Where we’re headed
- Empirical question: do P4P programs affect hospital prices?
- Why might we have an endogeneity problem here?
- What we need to answer this question:
- Hospital prices
- Penalty status
- Some “exogenous” source of variation in penalty status…