The Role of Physicians in Health Care Delivery
Why focus on physicians?
The U.S. spends heavily to train and employ physicians, and patients place enormous trust in them.
Yet, across markets, patients with the same condition can receive very different treatments.
Why do highly skilled professionals make such different choices?
And what does that mean for costs, quality, and equity?
Today’s Roadmap
- The structure of health care delivery
- How training, affiliations, and institutions shape practice
- Physicians as gatekeepers
- Why they hold outsized influence over patient care
- Physician agency
- Information, incentives, and alignment with patient interests
- Variation and waste
- Evidence from the Dartmouth Atlas and low-value care studies
Landscape of Health Care Delivery in U.S.
Lots of different players
- Physicians
- Nurses
- Hospitals
- Prescription drugs
- Rehabilitation (home health, SNF, rehab hospitals)
- Long-term care
- Ancillary services (labs, imaging)
But physicians have an outsized role, shaping nearly all areas of delivery.
Training and specialization
- Medical school, residency, fellowship shape practice styles
- Primary care vs. specialists
- Referral flows determine how patients move through the system
Organizational affiliations
- Self-employed solo practice
- Group practices
- Employment by hospitals or insurers
These affiliations influence autonomy, resources, and incentives.
Physician–hospital interactions
- General acute-care hospitals
- Rehabilitation hospitals
- Specialty centers (children’s, cardiac, cancer, orthopedic)
- Long-term care hospitals
- Outpatient vs. inpatient; stand-alone EDs and surgery centers
Ownership structures
- Government
- Private not-for-profit
- Private for-profit
- Private equity
Ownership affects institutional priorities and the constraints physicians face.
Physicians as Gatekeepers
Scope of influence
- Entry point for most patients (PCPs, ED)
- Referrals to specialists and ancillary services
- Specialists refer further, select surgery sites, order tests
- Hospitalists/specialists coordinate post-acute care
- All physicians help determine medications
Determinants of decisions
- Patient preferences and health needs
- Physician training and skillset
- Knowledge of available interventions
- Payment incentives
- Relationships with peers and institutions
Physician agency
- Physicians more informed than patients
- Physicians act as agents, making/suggesting care decisions
- Key question: Do these decisions align with what patients would choose under full information?
Variation in Utilization
Consequences of agency
- Patients experience physician-driven frictions and incentives
- Care depends on the physician’s practice style
- Leads to variation in utilization and spending across and within markets
- Example: Is Health Care Shoppable?
Variation raises the question: When is it waste?
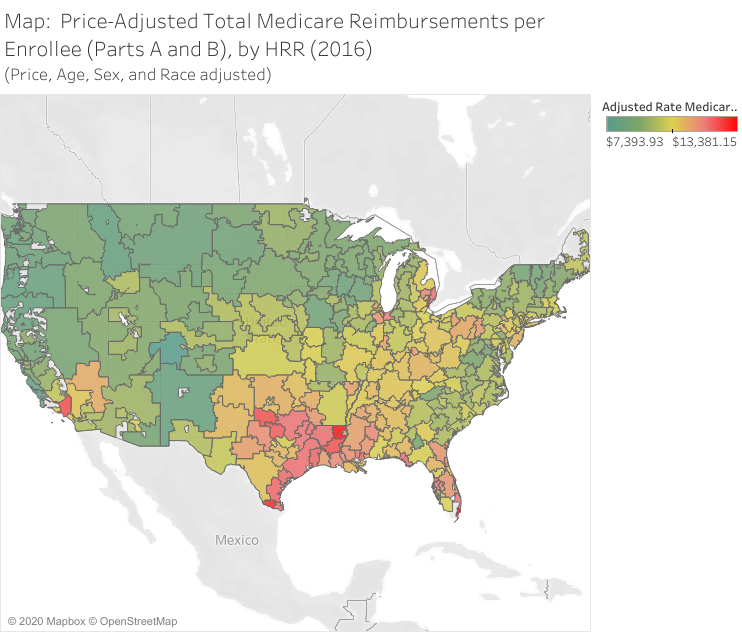
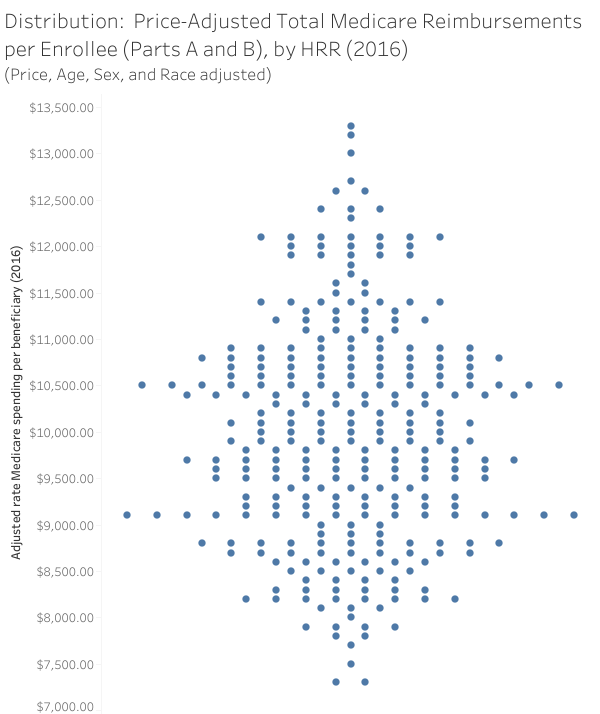
Variation versus Waste?
How much is waste?
- Over 30% of health care spending may be wasteful (The Atlantic, 2013)
Examples
- Payment quirks by location
- Advanced imaging with little benefit
- Proton therapy for some cancers
- Coronary stents for low-risk patients
- Arthroscopic knee surgery
But: waste is hard to identify prospectively.
See MIT report on end-of-life spending.